Knowledge hub

ICBC Physiotherapy: Accessing Treatment During your First 12 weeks of Recovery
Understanding how to access physiotherapy after a motor vehicle accident can significantly impact recovery outcomes. British Columbia's Enhanced Care system provides automatic pre-approval for 25 physiotherapy sessions during the first 12 weeks following a crash, removing administrative barriers and enabling immediate treatment access without physician referrals.
Key Takeaways
- Enhanced Care provides automatic pre-approval for 25 physiotherapy sessions within the first 12 weeks after any motor vehicle accident in BC
- Direct billing through ICBC's Recovery Network eliminates upfront costs when you provide your claim number and PHN
- The 12-week pre-approved period begins immediately upon crash occurrence, making early booking critical to maximize available sessions
- Extension requests should begin after the third treatment session and be submitted between sessions 7-9 to prevent treatment gaps
- Recovery specialists serve as your primary liaison and should be contacted every 2-3 weeks to expedite approvals and maintain treatment continuity
Table of Contents
- What's Covered Under ICBC's Enhanced Care for Physiotherapy
- How to Access Direct Billing and Payment
- Critical Timeline for Booking and Starting Treatment
- Extending Coverage Beyond 12 Weeks and Working with Recovery Specialists
What's Covered Under ICBC's Enhanced Care for Physiotherapy
ICBC's Enhanced Care system represents a fundamental shift in how physiotherapy coverage works for motor vehicle accident victims in British Columbia. Implemented in May 2021, this system provides automatic pre-approval for 25 physiotherapy sessions during the first 12 weeks following any crash. This coverage applies universally to all BC residents injured in motor vehicle accidents, regardless of who was at fault.

The financial structure of Enhanced Care establishes clear payment frameworks for different treatment types. Standard treatment sessions receive $95 per session, with rates updated as of May 1, 2025. These standard sessions must include a minimum of 20 minutes of one-on-one care between the physiotherapist and patient. This time requirement ensures that patients receive meaningful therapeutic intervention rather than superficial consultations.
Certain conditions and treatment scenarios qualify for non-standard prolonged sessions at $145 per session. These higher-rate sessions apply specifically to the following situations:
- Concussion and vestibular injuries requiring specialized treatment protocols
- Spinal cord injuries with complex rehabilitation needs
- Complex orthopedic conditions involving multiple body systems
- In-home or community-based treatment when patients can't access clinic facilities
Initial assessment visits receive separate coverage at $147 per visit, recognizing the additional time and documentation requirements for comprehensive evaluations. These assessments establish baseline measurements, identify functional limitations, and create treatment plans that guide the recovery process.
One of the most significant changes under Enhanced Care involves the recognition of physiotherapists as primary care practitioners. This designation eliminates the previous requirement for physician referrals during the initial 12-week period. Patients can now access physiotherapy immediately after a crash without waiting for medical appointments or referral paperwork. This direct access removes administrative barriers that previously delayed treatment initiation.
The rate increases effective May 1, 2025, result from five-year reviews mandated under the Insurance (Vehicle) Act. These reviews incorporate consultations with health care associations to ensure rates remain competitive and reflect current practice costs. For treatments administered on or after April 1, 2019, ICBC serves as the first payer, meaning physiotherapy expenses go through ICBC before any other insurance coverage.
This comprehensive coverage structure ensures that ICBC physiotherapy remains accessible and affordable during the critical early recovery phase. The system acknowledges that different injury types and severity levels require varying treatment intensities and durations.
How to Access Direct Billing and Payment
The ICBC Recovery Network streamlines the payment process for physiotherapy services through direct billing arrangements. When you visit a provider within this network during the pre-approved period, you pay nothing upfront. The clinic bills ICBC directly, eliminating the need for patients to manage reimbursement paperwork during their recovery.
Accessing these pre-approved treatments requires two essential pieces of information. You must provide your ICBC claim number and your Personal Health Number (PHN) to the physiotherapy clinic. The claim number generates automatically when you report the accident to ICBC, typically within hours of the initial report. This claim number serves as the primary identifier that links your treatment to your specific accident case.
Providers outside the Recovery Network may require upfront payment from patients. In these situations, you'll need to submit expenses through ICBC's claims process for reimbursement. These out-of-pocket expenses must be submitted within 180 days of when you incurred them. Missing this deadline can result in denial of reimbursement, leaving you financially responsible for treatment costs that would otherwise be covered.
Reimbursement amounts are limited to ICBC's approved rates, exclusive of any user fees that providers might charge above these rates. When providers charge more than ICBC's approved rates, extended health coverage through employers or private insurance can cover these additional user fees. This layered coverage approach ensures that patients aren't disadvantaged by choosing providers who charge premium rates for specialized services.
Direct deposit provides the fastest reimbursement method for out-of-pocket expenses. Setting up direct deposit with ICBC accelerates the payment timeline significantly compared to waiting for mailed checks. This speed becomes particularly important when managing multiple treatment sessions over several weeks.
Healthcare providers face their own submission requirements. Provider invoices must be submitted within 45 days of treatment provision. These invoices must be billed under the name of the practitioner who actually provided the service, not under another practitioner's credentials or clinic name. Late submissions may be denied at ICBC's discretion, creating potential payment disputes that complicate the treatment relationship.
Special circumstances affect payment priority. For workplace injuries, WorkSafeBC takes precedence as the primary payer, with ICBC serving as secondary coverage. This hierarchy matters because WorkSafeBC may cover different services or apply different approval criteria than ICBC. For medical equipment expenses incurred on or after May 1, 2025, ICBC serves as the first payer, simplifying the claims process for devices like braces, supports, or home therapy equipment.
The direct billing system within the Recovery Network eliminates financial stress during recovery. Patients can focus on physiotherapy treatment without worrying about upfront costs or reimbursement paperwork. This financial accessibility ensures that economic concerns don't delay or prevent necessary treatment during the critical first 12 weeks.
Critical Timeline for Booking and Starting Treatment
The 12-week pre-approved period begins immediately upon crash occurrence, not when you report the claim or book your first appointment. This distinction creates a critical urgency for accident victims. Every day of delay reduces the total benefit available during this crucial early recovery phase. A person who waits two weeks before booking their first physiotherapy appointment effectively has only 10 weeks remaining in their pre-approved period.
Booking appointments as soon as possible maximizes both the therapeutic benefit and the practical value of the pre-approved coverage period. Research consistently demonstrates that early intervention improves recovery outcomes and reduces the likelihood of developing long-term complications. Acute injuries respond better to treatment when physiotherapy begins within the first few days after the crash. Delayed treatment initiation allows inflammation to persist, range of motion to decrease, and compensatory movement patterns to develop.
Reporting your claim as soon as safely possible expedites treatment authorization. While the claim number generates quickly after reporting, any delay in reporting delays your ability to provide this essential information to physiotherapy clinics. The direct access to physiotherapy without physician referrals during the initial 12-week period represents a significant advantage, but only if you take immediate action to begin treatment.
The chronic pain development risk increases substantially with treatment delays. Acute pain that persists beyond normal healing timelines can transform into chronic pain syndromes that prove far more difficult to treat. The first 12 weeks represent a critical window when appropriate intervention can prevent these long-term complications.
Strategic planning for coverage extensions should begin early in the treatment process. Extension requests should begin after the third treatment session, with formal submissions occurring between treatments 7-9. This timing isn't arbitrary. It provides enough treatment history to demonstrate medical necessity while allowing sufficient processing time before the 25 sessions expire.
ICBC's approval processing times vary based on provider network status. Recovery Network providers receive decisions within a minimum of two weeks. Non-network providers face longer waits, up to 20 business days for extension approvals. These processing times can create treatment gaps if requests aren't submitted strategically. A patient who waits until session 23 to request an extension might face a two-week gap without coverage while waiting for approval.
Treatment gaps compromise recovery progress in multiple ways. Therapeutic gains achieved through consistent treatment can diminish during interruptions. Inflammation may increase, range of motion may decrease, and pain levels may escalate. These setbacks require additional sessions to regain lost ground, effectively wasting limited coverage resources.
The timeline pressure affects treatment intensity and frequency decisions. Patients with severe injuries might benefit from three sessions per week during the acute phase, consuming their 25 sessions within approximately eight weeks. This aggressive treatment schedule can produce superior outcomes for appropriate cases, but it requires even more careful planning for extension requests. Less severe injuries might respond adequately to two sessions per week, spreading the 25 sessions across the full 12 weeks.
Calendar awareness becomes essential for maximizing benefits. Consider holidays, scheduled vacations, or other commitments that might interrupt treatment schedules. A patient who plans a two-week vacation at week six should account for this interruption when planning treatment frequency. The 12-week clock continues running regardless of treatment interruptions.
For those with questions about timing or coverage specifics, comprehensive information resources exist. The frequently asked questions section addresses common concerns about booking timelines and treatment planning. These resources help patients make informed decisions about when and how frequently to schedule sessions.
Extending Coverage Beyond 12 Weeks and Working with Recovery Specialists
Most motor vehicle accident injuries heal within 12 weeks, but certain conditions require extended treatment periods. Healthcare providers must demonstrate medical necessity for additional treatments beyond the initial pre-approved period. This demonstration requires more than simple statements that treatment should continue. Providers must present objective evidence of ongoing impairment, document functional improvements achieved through treatment, and provide clinical rationale for why additional sessions will produce further gains.
ICBC assigns recovery specialists as your primary liaisons throughout the claims and recovery process. These specialists serve as the connection point between patients, healthcare providers, and the insurance system. Their role extends beyond simple claims processing. Recovery specialists coordinate multiple aspects of care, from treatment approvals to equipment authorization to rehabilitation planning.
Proactive communication with recovery specialists significantly impacts treatment continuity. I recommend contacting your recovery specialist every 2-3 weeks, even when recovery is progressing smoothly. These regular check-ins keep specialists informed about your treatment progress, build rapport that facilitates approvals, and identify potential issues before they create coverage gaps. Many patients make the mistake of contacting recovery specialists only when problems arise, missing opportunities to establish positive working relationships.
Regular communication serves multiple strategic purposes. Recovery specialists manage numerous cases simultaneously, and frequent contact ensures your case remains on their radar. When extension requests arrive from patients who've maintained consistent communication, specialists already understand the treatment context and can process approvals more efficiently. This familiarity can mean the difference between rapid approval and extended review periods.
Complex cases may require Comprehensive Medical Assessments (CMAs) conducted by independent healthcare professional teams. These CMAs provide objective evaluation of injuries and recommend appropriate benefits for continued recovery. While some patients view CMAs with apprehension, these assessments often work in the patient's favor by documenting injury severity and treatment needs that might not be fully apparent from clinical notes alone.
Processing times for extensions follow the same network-dependent timeline as initial approvals. Recovery Network providers receive decisions within approximately two weeks. Non-network providers face up to 20 business days for extension processing. These timelines underscore the importance of submitting extension requests between sessions 7-9, well before the pre-approved sessions expire.
Healthcare providers must maintain detailed treatment records to support extension requests. These records should include objective measures of progress such as range of motion measurements, strength testing results, and functional capacity evaluations. Subjective improvements like pain reduction matter, but objective data carries more weight in approval decisions. Documentation should also address functional improvements in activities of daily living, work capacity, and recreational activities.
The clinical rationale for continued treatment must address specific questions. What goals remain unmet? What functional limitations persist? How will additional treatment sessions address these remaining issues? What expected timeline exists for achieving treatment goals? Vague statements about ongoing pain or general need for continued care rarely satisfy approval requirements.
Non-standard treatment applications require completion of specific forms, particularly Form CL752 with detailed justification. This form requests information about why prolonged sessions are medically necessary, what specific interventions require extended time, and how these interventions relate to the motor vehicle accident injuries. Incomplete or insufficiently detailed forms result in delays or denials that interrupt treatment continuity.
Standard treatments must meet minimum time requirements of 20 minutes of one-on-one patient care for full reimbursement. This requirement prevents billing for brief check-ins or primarily equipment-based treatments with minimal direct therapist involvement. Providers who don't meet these minimum time requirements risk payment disputes that can complicate the treatment relationship.
Advanced recovery specialists provide specialized expertise for severe, permanent, or catastrophic injuries. These specialists coordinate lifetime care provisions, home modifications, comprehensive rehabilitation services, and long-term treatment planning. Cases involving spinal cord injuries, traumatic brain injuries, or multiple severe fractures typically warrant assignment to advanced specialists who understand the complex, long-term needs these injuries create.
The extension system recognizes individual variability in healing timelines. While most injuries resolve within 12 weeks, factors like age, pre-existing conditions, injury severity, and treatment adherence affect recovery rates. A 65-year-old with osteoarthritis who suffers multiple rib fractures will likely require longer treatment than a 25-year-old with a simple whiplash injury. The system provides flexibility to accommodate these individual differences through the extension process.
Documentation strategy should begin from the first treatment session. Providers who anticipate potential extension needs should establish baseline measurements comprehensively and document progress consistently throughout treatment. This documentation creates a clear narrative of injury severity, treatment response, and ongoing needs that supports extension requests.
Patients can advocate for themselves within the extension process. While healthcare providers submit the formal requests, patient input about functional limitations and treatment benefits adds valuable context. If you're struggling with work duties, household tasks, or self-care activities due to persistent symptoms, communicate these challenges clearly to both your physiotherapist and recovery specialist.
The extension approval process isn't adversarial by design. ICBC's stated goal involves supporting recovery and return to pre-accident function. However, the system requires objective evidence and clear justification to ensure treatment remains medically necessary and cost-effective. Meeting these requirements protects both the sustainability of the Enhanced Care system and the legitimacy of extension requests.
Recovery doesn't follow a uniform timeline or predictable path. The 12-week pre-approved period covers most cases, but the extension process ensures that individuals with complex or severe injuries receive the treatment they need. Understanding how to work effectively with recovery specialists and document treatment needs positions you to access continued coverage when medically justified.
If you've been involved in a motor vehicle accident and need immediate access to physiotherapy, don't wait for the 12-week clock to run down. Early treatment produces better outcomes, and every pre-approved session you don't use is a lost opportunity for recovery. Book your initial assessment today and begin your recovery journey with experienced professionals who understand the ICBC system and can maximize your benefits while delivering evidence-based treatment that supports your return to full function.
Announcements & Updates

Accessories Available to Help You Recover
Accessories Available to Help You Recover
Recovery doesn't stop when you leave our clinic. We've carefully selected four essential accessories that extend your treatment benefits into your daily routine. Each tool has been chosen for its effectiveness in supporting rehabilitation and preventing re-injury.
These accessories are the same professional equipment we recommend during your sessions. By making them available at our front desk, we've eliminated the guesswork of shopping online and ensured you're getting exactly what your body needs for optimal recovery.
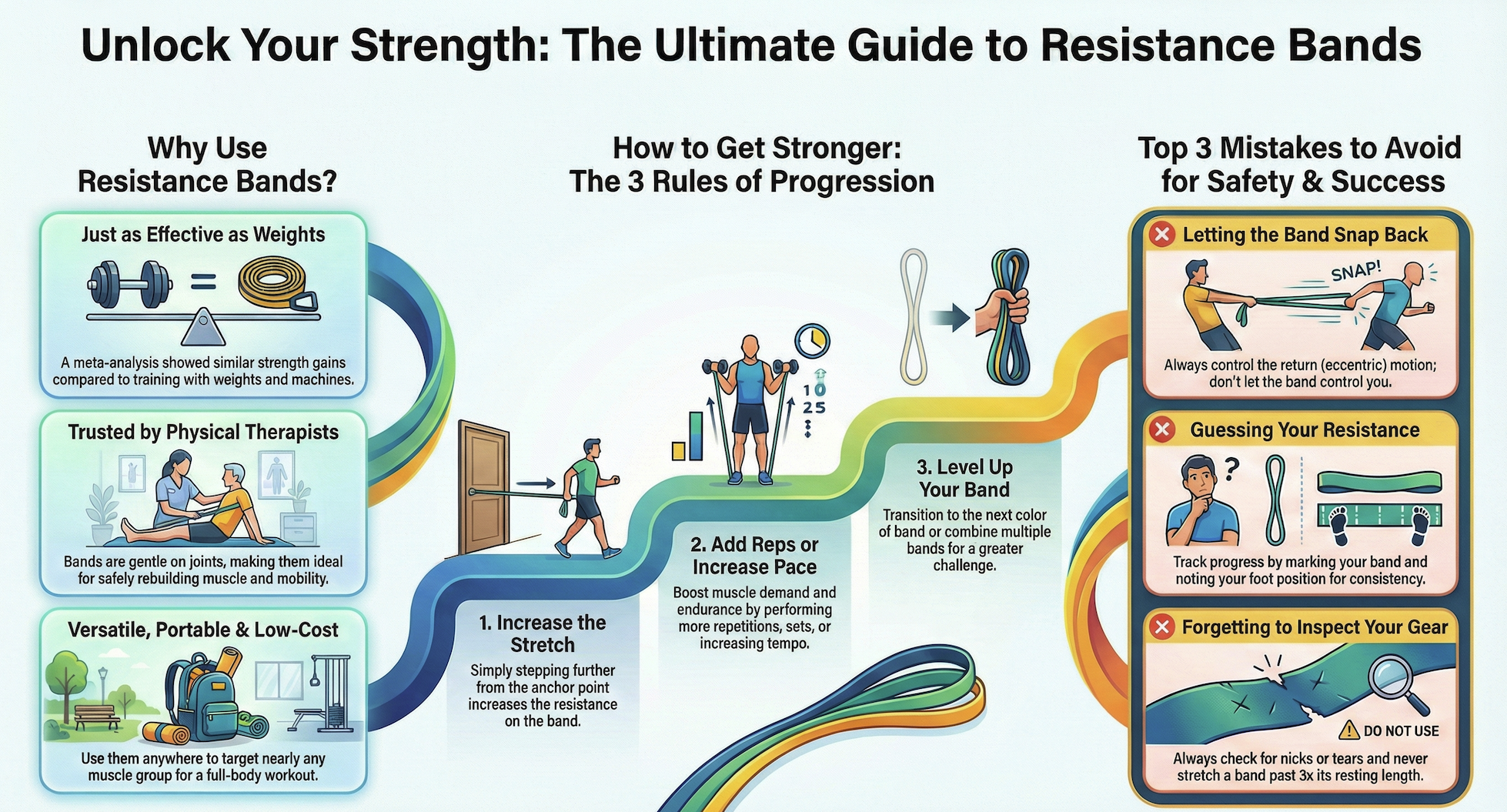
How Resistance Bands Build Strength

The Resistance Band Set (5-Pack) is available for $19.99 and includes five progressive resistance levels. This allows you to gradually increase difficulty as your strength returns, making it perfect for post-injury strengthening and mobility work. Starting with lighter resistance and progressing to heavier bands ensures safe, controlled recovery.

Our 2-pack Stretching Bands cost $7.99 and focus on improving flexibility while preventing re-injury. Use them as part of your daily mobility routine or during warm-ups before exercise. Regular stretching with these bands helps maintain the gains you achieve during your clinic visits and keeps muscles supple between appointments.
Why Shoulder Pulleys Restore Mobility
The Shoulder Pulley System at $19.99 features an over-the-door design that requires no permanent installation. This makes it incredibly convenient for home use, allowing you to perform prescribed exercises in your own space. The pulley system is particularly effective for shoulder rehabilitation following injuries or surgeries.
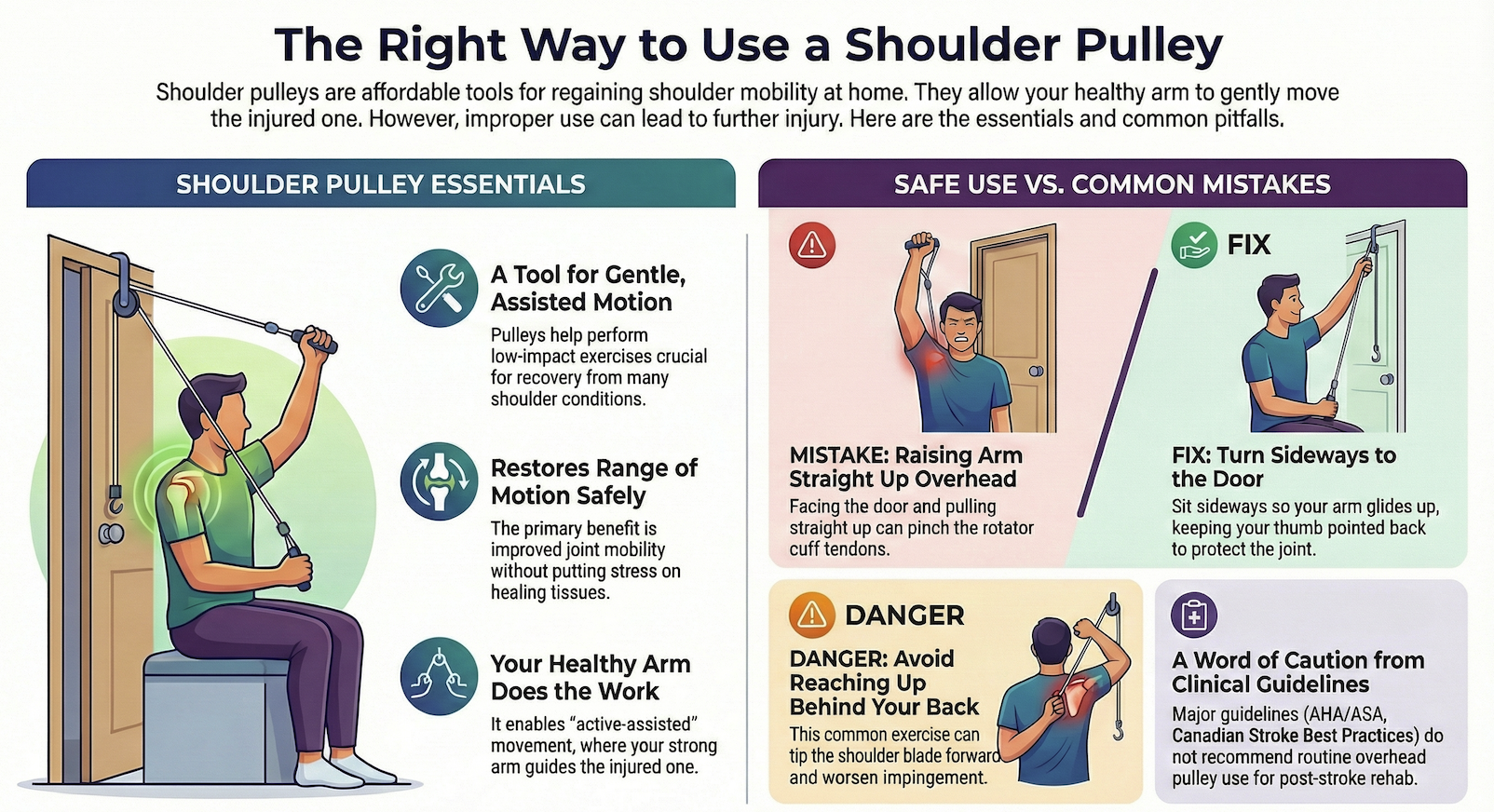
Range of motion exercises become much easier with this tool, helping you restore mobility faster. Our staff can demonstrate proper setup and exercise protocols during your visit, ensuring you're using the system correctly and safely at home.
When to Use Lacrosse Balls

Our Pressure Balls are priced at $9.99 and come in black or white options. These firm balls provide targeted myofascial release and trigger point therapy, allowing you to work out muscle knots and tight spots between appointments. They're small enough to take anywhere and can be used against a wall, on the floor, or even while sitting at your desk.
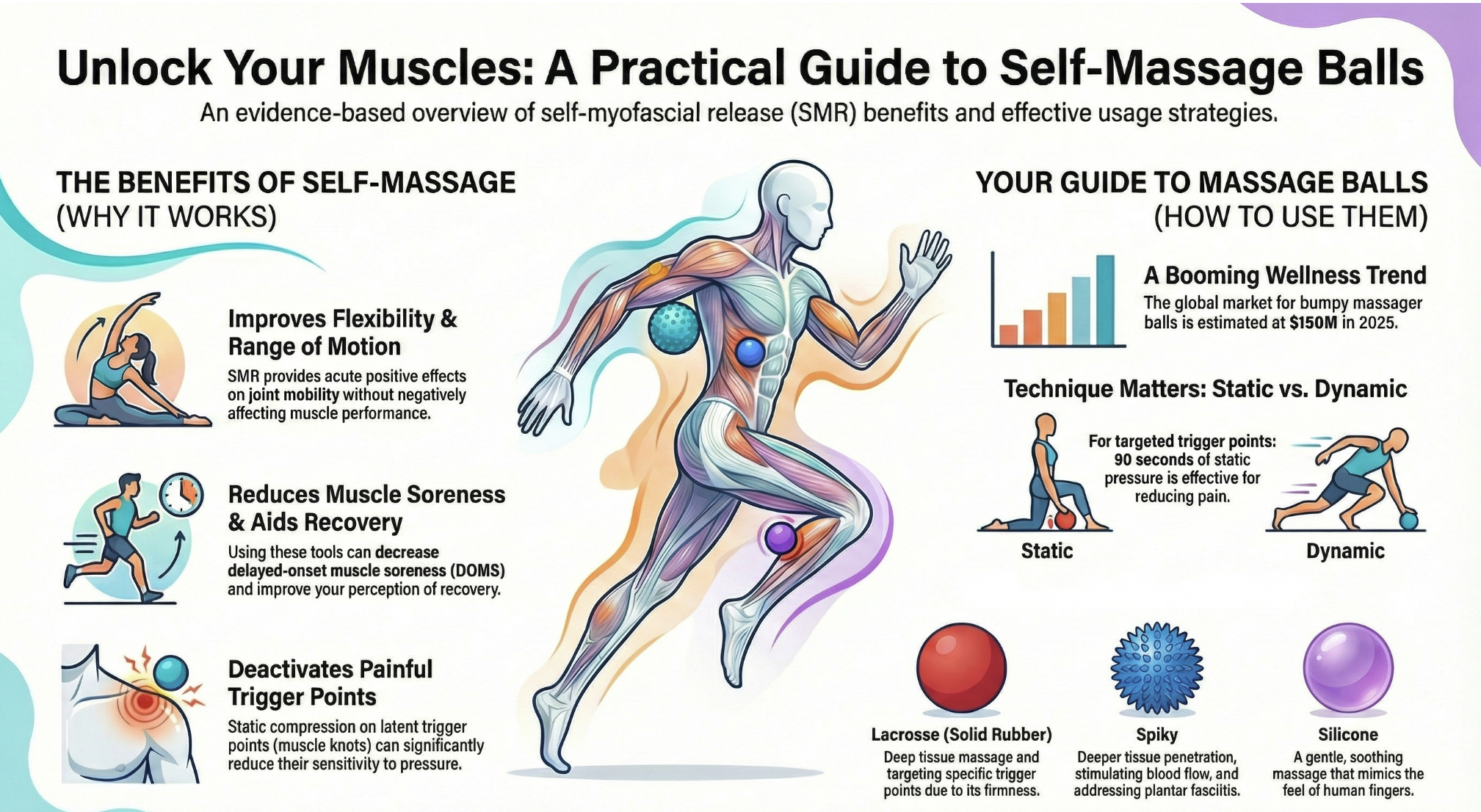
Self-massage with a Pressure ball helps maintain the muscular relief achieved during your treatments. Focus on areas that feel tense or restricted, applying gentle to moderate pressure and moving slowly across the muscle. Ask our front desk staff which accessories best suit your recovery needs, and we'll help you choose the right tools to support your healing journey.
Ready to enhance your recovery? Pick up the accessories you need during your next visit, or book an appointment today and speak with our team about which tools will help you heal faster.

Understanding Your Extended Health Benefits in BC
Key Takeaways
- Extended health benefits cover Physiotherapy and Registered Massage Therapy services beyond what provincial health insurance provides, with most plans offering annual maximums that expire at year-end.
- Direct billing simplifies the claims process by allowing our clinic to bill your insurance provider directly, eliminating paperwork and wait times for reimbursement.
- Your coverage includes advanced treatments like TMJ Physiotherapy, IMS, Shockwave Therapy, Headache Relief Treatment, and Vestibular and Concussion Physiotherapy.
- Unused benefits represent wasted money, as annual maximums reset at the end of your plan year and cannot be carried forward to the next year.
- Being proactive with coverage helps prevent future injuries and addresses minor issues before they become major problems requiring extensive treatment.
Table of Contents
- What Extended Health Benefits Cover in British Columbia
- Who Needs Extended Health Benefits and How to Access Them
- Maximizing Your Extended Health Benefits Coverage
- Understanding Costs and Limitations in BC
- Major Insurance Providers in British Columbia
- Direct Billing: Simplifying Your Benefits Experience
- Advanced Physiotherapy Treatments Covered by Your Plan
- The Cost of Not Using Your Benefits
What Extended Health Benefits Cover in British Columbia
Extended health benefits function as supplementary health insurance that goes beyond what provincial health insurance provides. While basic coverage addresses emergency care and physician visits, extended benefits fill the gaps for services like Physiotherapy and Registered Massage Therapy. These paramedical services represent some of the most valuable components of any extended health plan, particularly for BC residents dealing with chronic pain, sports injuries, or workplace-related musculoskeletal conditions.
Coverage varies significantly between different plans. Some employers offer comprehensive benefits with high annual maximums, while others provide basic coverage with lower limits. Most plans include annual maximums for specific categories, such as $500 to $1,500 per year for massage therapy or $500 to $2,000 annually for physiotherapy services. Understanding these limits becomes essential for planning your care throughout the year.
The structure of your benefits package typically includes several key elements:
- Annual maximums per service category that reset at the end of your plan year
- Coverage percentages, commonly ranging from 80% to 100% of treatment costs
- Per-visit or per-session limits for individual treatments
- Potential deductibles that must be met before coverage begins
What many people don't realize is that their paramedical services coverage extends to advanced treatment modalities. Your plan likely covers more than just basic physiotherapy sessions, including specialized treatments that address complex conditions requiring focused intervention approaches.
Who Needs Extended Health Benefits and How to Access Them
BC residents relying solely on provincial coverage face significant gaps in their healthcare needs. Provincial insurance doesn't cover Physiotherapy or Registered Massage Therapy for most conditions, leaving patients to pay out-of-pocket for these essential services. Extended health benefits bridge this gap, making preventive care and injury rehabilitation accessible and affordable.
Most British Columbians access extended health benefits through employer-sponsored group plans. These represent the most cost-effective option since employers typically contribute toward premium costs and group rates provide better coverage at lower prices. However, employer plans aren't the only option available. Self-employed individuals, contract workers, and those whose employers don't offer benefits can explore several alternatives:
For those with access to employer benefits, enrollment usually occurs during onboarding or annual enrollment periods. Missing these windows can mean waiting another year to access coverage, so staying informed about enrollment deadlines protects your access to care.
Maximizing Your Extended Health Benefits Coverage
The end of the year brings an important deadline for anyone with extended health benefits. Most plans operate on a calendar year or anniversary year basis, meaning your annual maximums expire and reset at year-end. Any unused portion of your benefits doesn't carry forward; it simply disappears. This represents money you've already paid for through premiums but haven't utilized.
Tracking your benefit usage throughout the year prevents last-minute surprises. Most insurance providers offer online portals or mobile apps where you can monitor claims and remaining coverage. Setting reminders to check your balance quarterly helps you plan treatments strategically. If you discover unused benefits in the final months of the year, consider booking appointments for maintenance care, addressing minor discomfort before it escalates, or treating conditions you've been putting off.
If you're covered by multiple plans, such as your own and your spouse's, coordination of benefits allows you to maximize reimbursement. The primary plan pays first, then the secondary plan covers remaining eligible expenses up to 100% of the cost. This arrangement can eliminate out-of-pocket expenses entirely for covered services. Check out our frequently asked questions for more information about how we handle coordination of benefits.
Major Insurance Providers in British Columbia
Navigating the insurance landscape becomes easier when you have direct contact information for major providers. Below you'll find details for the primary extended health insurance companies serving BC residents:
Pacific Blue Cross
Website: www.pac.bluecross.ca
Phone: 1-888-275-4672
Hours: Monday to Friday, 8:00 AM to 8:00 PM (Pacific Time)
Manulife
Website: www.manulife.ca
Phone: 1-888-626-8543
Hours: Monday to Friday, 8:00 AM to 8:00 PM (Eastern Time)
Sun Life Financial
Website: www.sunlife.ca
Phone: 1-800-361-6212
Hours: Monday to Friday, 8:00 AM to 8:00 PM (Eastern Time)
Canada Life
Website: www.canadalife.com
Phone: 1-800-724-3402
Hours: Monday to Friday, 8:00 AM to 8:00 PM (Eastern Time)
Green Shield Canada
Website: www.greenshield.ca
Phone: 1-888-711-1119
Hours: Monday to Friday, 8:00 AM to 8:00 PM (Eastern Time)
If you have coverage through a provider not listed here, call us to verify whether we can provide direct billing services for your specific plan. We work with numerous insurance companies and regularly add new billing relationships to better serve our patients.
Direct Billing: Simplifying Your Benefits Experience
Direct billing transforms how you access covered healthcare services. Instead of paying for treatments and waiting for reimbursement, our clinic bills your insurance provider directly. This arrangement offers several significant advantages that make accessing care simpler and more convenient.
The traditional claims process requires you to track receipts, complete claim forms, submit documentation, and wait weeks for reimbursement. Direct billing eliminates these steps entirely. You simply provide your insurance information at check-in, and we handle the rest. The insurance company receives the claim electronically, processes it, and pays us directly for the covered portion of your treatment.
We offer direct billing for most major insurance providers in British Columbia. Our administrative team stays current on insurance requirements, billing codes, and documentation standards to ensure smooth claim processing. If you're unsure whether we can provide direct billing for your specific plan, contact us before your appointment and we'll verify your coverage details.
Advanced Physiotherapy Treatments Covered by Your Plan
Your extended health benefits cover more than standard physiotherapy sessions. Most insurance plans include coverage for advanced treatment modalities that address complex conditions requiring specialized approaches. Understanding the full scope of your coverage helps you access the most appropriate care for your specific condition.
TMJ Physiotherapy treats temporomandibular joint disorders that cause jaw pain, clicking, limited mouth opening, and headaches. This specialized treatment combines manual therapy techniques, exercises, and education to address the jaw joint and surrounding muscles. Many patients don't realize their benefits cover this treatment, continuing to suffer with jaw pain that responds well to physiotherapy intervention.
IMS Physiotherapy, or Intramuscular Stimulation, uses thin needles to treat muscle tension and nerve irritation causing chronic pain. This technique proves particularly effective for conditions that haven't responded to other treatments. While similar in appearance to acupuncture, IMS follows a different treatment philosophy based on Western medical principles and neurophysiology. Your extended health benefits typically cover IMS under your physiotherapy allocation.
Shockwave Therapy delivers acoustic waves to injured tissues, stimulating healing in chronic conditions like plantar fasciitis, tennis elbow, and calcific tendonitis. This advanced treatment option accelerates recovery in conditions that often resist conventional therapy approaches. The technology costs thousands of dollars to acquire and maintain, making access through your insurance benefits particularly valuable.
Headache Relief Treatment addresses the musculoskeletal components contributing to tension headaches, migraines, and cervicogenic headaches. Physiotherapists assess neck alignment, muscle tension, posture, and movement patterns that trigger or worsen headaches. Treatment combines manual therapy, specific exercises, and ergonomic modifications. For chronic headache sufferers, this approach often reduces headache frequency and intensity significantly.
Vestibular and Concussion Physiotherapy treats dizziness, balance problems, and post-concussion symptoms. Specialized assessment identifies the specific systems affected by your condition, whether vestibular organs, visual tracking, or cervical spine issues. Treatment protocols retrain these systems, reducing symptoms and improving function. This specialized service requires advanced training and certification, yet remains covered under your physiotherapy benefits.
These advanced treatments appear on our services page, where you can learn more about each approach and the conditions they address. Don't assume your coverage only extends to basic treatments. Your benefits invest in evidence-based care that produces meaningful results, regardless of the technique required.
The Cost of Not Using Your Benefits
Leaving extended health benefits unused represents a genuine financial loss. You've paid for this coverage through premiums, whether directly or as part of your employment compensation package. When annual maximums expire unused, you've essentially donated money to your insurance company without receiving any value in return.
Consider the mathematics. If your plan provides $1,000 in annual physiotherapy coverage and you use none of it, you've lost access to $1,000 worth of care. For a family with multiple covered members, unused benefits can represent several thousand dollars in forfeited healthcare services. This becomes particularly significant when you consider that most people could benefit from preventive or maintenance care even if they're not currently injured.
Beyond the immediate financial loss, unused benefits represent missed opportunities for prevention. Physiotherapy isn't only for treating existing injuries. It identifies movement dysfunctions, muscle imbalances, and biomechanical issues that increase injury risk. Addressing these factors before they cause problems prevents the pain, disability, and extended treatment that major injuries require. You might visit the dentist twice yearly for preventive care; your musculoskeletal system deserves similar attention.
Taking a proactive approach to benefit usage supports long-term health. That minor shoulder discomfort you've been ignoring? It might respond quickly to a few physiotherapy sessions now, preventing it from becoming a frozen shoulder requiring months of treatment later. The occasional low back stiffness you experience? Early intervention can prevent it from progressing to debilitating pain that interferes with work and daily activities.
Registered Massage Therapy offers similar preventive value. Regular treatments reduce muscle tension, improve circulation, decrease stress, and maintain flexibility. Athletes use massage to support training and prevent overuse injuries. Office workers benefit from addressing the postural strain of desk work before it causes chronic pain. Your benefits make these preventive treatments accessible and affordable.
The end of the year creates urgency around benefit usage, but this shouldn't be your only consideration. Year-round benefit utilization spreads your care throughout the year, supporting consistent health maintenance rather than rushed appointments in December. However, if you're reading this in the final months of the year with unused benefits remaining, scheduling appointments now prevents leaving money on the table.
Check our pricing information to understand how your coverage applies to different services and treatment durations. This transparency helps you plan your benefit usage strategically, maximizing the value you receive from your insurance coverage.
Ready to maximize your extended health benefits before they expire? Our team specializes in Physiotherapy and Registered Massage Therapy with direct billing for most major insurance providers. Book your appointment today and put your benefits to work improving your health. Don't leave money on the table by letting your coverage go unused this year. Schedule now while appointment availability remains.

10/10/25 Update: Gift Cards Now Available
TL;DR
- Gift cards are available for purchase starting today at our front desk or through the blvdwellness.janeapp.com/myaccount
- Cards have no expiration dates or hidden fees and can be used toward any of our services
- Digital gift cards offer last-minute gifting solutions with immediate or scheduled email delivery
Update Overview
Gift Cards Now Available
Gift card options that make perfect presents for any occasion. The holiday season is approaching quickly, and these cards provide a convenient solution for thoughtful gift-giving. Beyond the holidays, they're ideal for birthdays, anniversaries, or even spontaneous gestures when you want to show someone you care about their wellbeing.

How to Purchase Gift Cards
We've made purchasing simple with two convenient options. Physical gift certificates are available at our front desk during regular business hours, while digital gift cards can be purchased online through blvdwellness.janeapp.com/myaccount
Here's how to purchase based on your preferred method:
- Physical certificates: Visit our front desk and speak with our reception staff, who will process your purchase and provide a beautiful certificate ready for gifting
- Digital gift cards: Log into blvdwelllness.janeapp.com, navigate to the gift card section on the left panel, select your desired amount, and complete the checkout pro

Digital cards are delivered via email, so you can send them immediately for last-minute gifts or schedule delivery for a specific date in the future.
Why Choose Our Gift Cards
Our gift cards come with benefits that make them stand out from typical gift options. Recipients can use them toward any of our available services, giving them complete freedom to choose what best supports their wellness journey. You won't find expiration dates or hidden fees attached to our cards, and we offer flexible denominations to fit any budget.
The digital option provides a particularly convenient solution when you need a thoughtful gift quickly. Life gets busy, and sometimes special occasions sneak up on us, but you can still give a meaningful and practical gift within minutes.
Start Shopping Today
Don't wait until the last minute to prepare for upcoming celebrations and special occasions. Our front desk staff are ready to answer any questions you have about gift card options, denominations, or the purchasing process. Buying gift cards now means you'll be prepared whenever a gifting opportunity arises.
Ready to give the gift of wellness? Visit our front desk during your next appointment or purchase digital gift cards online today through our JaneApp. Your loved ones will appreciate the thoughtfulness, and you'll appreciate the convenience.
